SPROTTE® - Safety Revolution in Spinal Anesthesia
The unique design of the Sprotte needle has made it a success. This design has revolutionized spinal anesthesia. PAJUNK® is proud to have taken this step together with Prof. Sprotte.
Milestones of the Sprotte:
1979 - Launch
1980 - break trough in regional anesthesia
In 1980’s - First studies confirming the concept of the Sprotte needle repeatedly. Thus increasing interest.
1990 - Scientific success of the needle - first comparative studies with Quincke & Whitacre needle. This led to the Sprotte needle with its atraumatic tip geometry becoming the new standard in anesthesia in some parts of the world market.
However, what is so revolutionary about our Sprotte?
Atraumtic Tip Design
The ogive shaped tip significantly reduces the risk of PDPH³ and the rounded edges of the lateral eye minimize trauma to the dura mater. Thanks to the tip, design there is a consistent tactile feedback.
Lateral Eye
- The burr-free, rounded atraumatic edges optimizes the gliding properties. Additional there is a minimum chance of tissue coring and carry-over into the subarachnoid space
Optimal Lateral Eye Size and Placement
- The Sprotte has an unobstructed backflow, even if the eye is partially blocked by the arachnoid membrane. This allows a quicker CSF flashback1
Precision-Ground Metal Stylet
- The stylet closes the lateral eye precisely to minimise chance of tissue coring.² Further the polished, rounded tip of the stylet prevents abrasion on the inner needle tube.
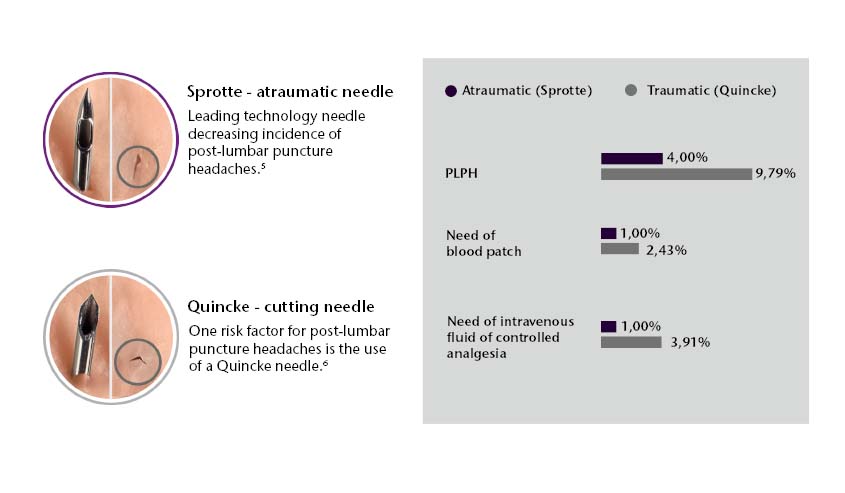
Further, the Sprotte needle has also revolutionized the lumbar puncture area.
In comparison with the Quincke tip needles, the Sprotte needles has an Evidence class 1, recommendation level A8,9,10,11 in the sector of lumbar puncture.
The conclusion out of different studies: “It’s time to change the needle.”4,5,14 for lumbar puncture.
- Atraumatic lumbar puncture needles are safe to use4,5,7,8,9,10,11
- Require a minimal learning curve8
- Provide reliable results9
- Minimize side effects, complications, and recovery time5
- High savings potential by minizing process and treatment costs6,11
- Increase efficiency6
1 Saenghirunvattana R. et al. A comparison study between newly-designed pencil-point and cutting needles in spinal anesthesia, J. Med. Assoc. Thai. 2008; 91 (Suppl 1): S156–161
2 Armon C., Evans R. W. Addendum to assessment: Prevention of postlumbar puncture headaches Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology., Neurology., 2005; 65; 510
3 Cesarini, M. et al. Sprotte needle for intrathecal anaesthesia for Caesarean section: incidence of postdural puncture headache., Aaesthesia 1990; 45: 646–658
4Davis, A.; Dobson, R.; Kaninia, S.; Giovannoni, G.; Schmierer, K. (2016): Atraumatic needles for lumbar puncture: why haven't neurologists changed? In Practical neurology 16 (1), pp. 1822. DOI: 10.1136/practneurol-2014-001055.0
5 Engedal, Thorbjørn S.; Ørding, Helle; Vilholm, Ole Jakob (2015): Changing the needle for lumbar punctures: results from a prospective study. In Clinical neurology and neurosurgery 130, pp. 7479. DOI: 10.1016/j.clineuro.2014.12.020.
6 Tung, C. E.; Yuen, T. S.; Lansberg, M. G. (2012): Cost comparison between the atraumatic and cutting lumbar puncture needles. In Neurology 78, pp. 109113.
7 Arevalo-Rodriguez, Ingrid; Muñoz, Luis; Godoy-Casasbuenas, Natalia; Ciapponi, Agustín; Arevalo, Jimmy J.; Boogaard, Sabine; Roqué I Figuls, Marta (2017): Needle gauge and tip designs for preventing post-dural puncture headache (PDPH). In The Cochrane database of systematic reviews 4, CD010807. DOI: 10.1002/14651858.CD010807.pub2.
8 McLaughlin, Colleen A.; Hockenberry, Marilyn J.; Kurtzberg, Joanne; Hueckel, Rémi; Martin, Paul L.; Docherty, Sharron L. (2014): Standardization of health care provider competencies for intrathecal access procedures. In Journal of pediatric oncology nursing: official journal of the Association of Pediatric Oncology Nurses 31 (6), pp. 304316. DOI: 10.1177/1043454214543019.
9 Nath, Siddharth; Koziarz, Alex; Badhiwala, Jetan H.; Alhazzani, Waleed; Jaeschke, Roman; Sharma, Sunjay et al. (2018): Atraumatic versus conventional lumbar puncture needles: a systematic review and meta-analysis. In The Lancet 391 (10126), pp. 11971204. DOI: 10.1016/S0140-6736(17)32451-0.
10 Rochwerg, Bram; Almenawer, Saleh A.; Siemieniuk, Reed A. C.; Vandvik, Per Olav; Agoritsas, Thomas; Lytvyn, Lyubov et al. (2018): Atraumatic (pencil-point) versus conventional needles for lumbar puncture: a clinical practice guideline. In BMJ, k1920. DOI: 10.1136/bmj.k1920.
11 Zhang, Yi C.; Chandler, Alexander J.; Kagetsu, Nolan J. (2014): Technical compliance to standard guidelines for lumbar puncture and myelography: survey of academic neuroradiology attendings and fellows. In Academic radiology 21 (5), pp. 612616. DOI: 10.1016/j.acra.2014.01.021.
12 Bellamkonda, Venkatesh R.; Wright, Thomas C.; Lohse, Christine M.; Keaveny, Virginia R.; Funk, Eric C.; Olson, Michael D.; Laack, Torrey A. (2017): Effect of spinal needle characteristics on measurement of spinal canal opening pressure. In The American journal of emergency medicine 35 (5), pp. 769772. DOI: 10.1016/j.ajem.2017.01.047.
13 Puolakka, R.; Andersson, L. C.; Rosenberg, H. (2000): Microscopic Analysis of Threee Different Spinal Needle Tips After Experimental Subarachnoid Puncture. In Regional Anesthesia and Pain Medicine 25 (2), pp. 163169.
14 Lavi R., Rowe J.M., Avivi I. Lumbar Puncture. It Is Time to Change the Needle, Eur Neurol, 2010; 64:108113
Take a look at our Sprotte portfolio."